Health insurance coverage in the U.S. has expanded in recent years, yet a significant insurance gap remains. Thanks to the Affordable Care Act (ACA) and pandemic-era measures, the uninsured rate fell to around 8% of Americans in 2023 – roughly 26 million people, about half the rate before the ACA. However, simply having insurance is no guarantee of affordable healthcare. As of 2024, nearly one in four working-age adults was considered underinsured, meaning they technically had coverage but still faced prohibitively high medical costs. In other words, millions are “insured, but not protected” – a troubling reality that hits certain income groups and age brackets harder than others.
What Does It Mean to Be Underinsured?
Being underinsured means your health insurance fails to provide adequate financial protection. In policy terms, an underinsured person is usually someone who has insurance yet must pay so much out-of-pocket for care that it strains their budget or leads them to forgo needed care. The Commonwealth Fund, which regularly surveys U.S. households, defines an adult as underinsured if any of the following apply:
- High medical spending relative to income: Over the past year, your out-of-pocket health costs (excluding premiums) were ≥ 10% of your household income (or ≥ 5% if your income is low, under about 200% of the federal poverty level).
- High deductible relative to income: Your health plan’s annual deductible – the amount you must pay yourself before insurance pays – is ≥ 5% of your household income.
These criteria reflect a simple reality: if you’re spending a large share of your earnings on deductibles, copays, and other medical bills, your insurance isn’t truly affordable. Underinsured individuals often hesitate to seek care despite being “insured,” because the cost burden feels similar to being uninsured. For example, an underinsured patient might skip doctor visits or treatments knowing they’d have to pay thousands out-of-pocket due to a high deductible. In 2024, a survey found 57% of underinsured adults avoided necessary medical care because of the cost – a rate even higher than among the uninsured. In short, underinsurance translates to inadequate access to care, significant financial strain, or both, even though one technically has coverage.
Underinsurance in America: The Big Picture
How big is the underinsurance problem? Recent data show that roughly 23% of U.S. adults aged 19–64 were insured all year but met the underinsured criteria. This is in addition to those who were outright uninsured or had short coverage gaps. When combined, about 43% of working-age Americans experienced either a period of being uninsured or were underinsured over the past year – a sizable health insurance gap.
One reason underinsurance has become more common is the prevalence of plans with high deductibles and cost-sharing. Many employers have shifted toward high-deductible health plans, and individuals buying coverage on ACA marketplaces often choose plans with lower premiums but higher out-of-pocket costs. In 2022, nearly 29% of people with employer-sponsored insurance were underinsured, and the situation was even worse for those who purchased their own insurance on the individual market or ACA exchanges (about 44% underinsured). Even some Medicaid enrollees and Medicare beneficiaries on fixed incomes struggle with cost exposures (for instance, Medicare often requires supplemental plans to cap out-of-pocket expenses). The bottom line is that having insurance isn’t a binary yes/no anymore – the quality and comprehensiveness of that coverage matters hugely for affordability.
Who, then, are the underinsured? Let’s explore how underinsurance breaks down by income level and age group, since these factors are strongly linked to the adequacy of one’s coverage.
Underinsured by Income: Low and Middle-Income Americans at Risk
Income is one of the clearest predictors of underinsurance. Generally, lower-income Americans are far more likely to be underinsured than higher-income Americans. People with modest incomes often end up in health plans with higher relative cost burdens – whether through jobs that offer limited benefits or through marketplace plans that, even after subsidies, may carry sizable deductibles for silver or bronze-tier coverage.
According to a national survey, among adults under age 65 who had insurance all year, over one-quarter of those with low incomes were underinsured, versus only about one in ten of those with high incomes. The chart below illustrates underinsured rates by income bracket:
Below 133% of the federal poverty level: Approximately 26% of adults in this group were underinsured. Many in this bracket qualify for Medicaid (which generally has low out-of-pocket costs), but those who do not qualify or live in states with limited Medicaid expansion often end up with bare-bones private plans or go without needed care due to costs.
- 133–249% of poverty (just above poverty to modest income): Underinsurance peaks in this range at around 32%. This group may not qualify for Medicaid in some cases and often relies on ACA marketplace plans or less generous employer plans. Even after ACA subsidies, deductibles and copays can consume a significant portion of income in this bracket, leading to a high underinsured rate.
- Middle-income (250–399% of poverty): Underinsured rate about 24%. While better off than lower-income groups, many middle-income families still face high deductibles. They often earn too much to get the fullest ACA subsidies but not enough to comfortably handle thousands of dollars in cost-sharing if someone falls ill.
- High-income (400% of poverty and above): Underinsured rate drops to around 11%. Higher-income individuals and families can typically afford more comprehensive plans or absorb out-of-pocket costs more easily. In this group, underinsurance is relatively uncommon – roughly one in nine – though it does exist (for example, a high-earner might technically be “underinsured” if they chose a very high deductible plan, but they may be better positioned to pay those costs).
In summary, underinsurance disproportionately affects Americans of low and moderate income. Many in these income ranges face a tough trade-off: pay higher premiums for a more generous plan (which may be financially out of reach), or choose an affordable premium and risk large out-of-pocket expenses. The result is that millions of lower-income workers and families have coverage that meets legal standards but still leaves them financially vulnerable. One study found that households earning under about $50,000 were significantly more likely to carry medical debt or skip care due to cost, reflecting the burden of underinsurance on those least able to afford surprise bills
Underinsured by Age: Younger vs. Older Adults
Age is another important factor in the insurance gap. Different age groups encounter distinct coverage situations – from young adults just off their parents’ plans, to middle-aged people managing family healthcare costs, to older adults approaching Medicare eligibility. Broadly, older working-age adults (50–64) have the highest underinsured rates, while middle-aged and younger adults have slightly lower (but still significant) rates.
Younger Adults (19–34 years): This group – which includes older Gen Z and younger Millennials – had about a 23% underinsured rate as of 2022. Young adults benefited greatly from ACA provisions (like staying on a parent’s plan until 26 and Medicaid expansion in many states), which helped reduce uninsurance. However, those not on a parent’s plan often opt for the cheapest insurance available due to tight budgets, which can mean high deductibles. The result is nearly a quarter of young adults are underinsured. On the bright side, younger people tend to use less healthcare on average, so many might not hit their deductible in a given year – but if an accident or illness strikes, they may be unprepared for the costs.
Middle-Age Adults (35–49 years): This cohort – largely older Millennials and Gen X – had an underinsured rate around 20%. By this stage, many have families and more health needs, and while coverage rates are higher (most in this group have insurance through employers or ACA plans), cost exposure remains an issue for one in five. They often face the dual pressure of premiums and out-of-pocket costs, especially if covering spouses and children. Notably, many in this age range fall into the moderate-income category that, as noted above, sees high underinsured levels if their employer insurance is skimpy or if they buy insurance on their own.
Older Working-Age Adults (50–64 years): Americans in their late 50s to early 60s – predominantly late Gen X and Baby Boomers not yet eligible for Medicare – have the highest rate of underinsurance, about 27%. This means over one in four adults aged 50–64 with insurance still cannot afford needed care or bills. Several factors drive this: health needs generally increase with age, incomes may plateau or decline for some in this group (e.g. early retirees or those in transition), and individual insurance becomes pricier with age. Those who retire before 65 or lose jobs often have to find expensive private coverage (or COBRA), sometimes with high cost-sharing. Even in employer plans, older workers might utilize more services and more quickly reach a point where out-of-pocket costs accumulate. Unfortunately, this group must navigate a few years of potential underinsurance risk before Medicare kicks in at 65. It’s no surprise that many 60-somethings incur medical debt or skip treatments, given the cost pressures – among people 50–64 who were underinsured, a large share reported not filling prescriptions or foregoing care due to expense
It’s worth noting that Americans 65 and older are generally covered by Medicare, which dramatically lowers the uninsured rate in that age group. Medicare provides a baseline of coverage and caps hospital costs, but it does not cover everything (for instance, routine dental or long-term care are excluded, and prescription drug coverage comes via separate Part D or Advantage plans). Some seniors without supplemental insurance face high out-of-pocket costs for medications or services Medicare doesn’t fully cover. In that sense, underinsurance can affect seniors as well – for example, an older person on Medicare without a Medigap plan could be on the hook for 20% coinsurance indefinitely, potentially a large burden. However, by policy definition the term “underinsured” is usually analyzed for the under-65 population, since virtually all seniors have at least basic Medicare. The key generational takeaway is that younger generations (Gen Z, Millennials) have better coverage rates post-ACA than older generations did at the same age, but they now face a new challenge of inadequate coverage. Meanwhile, many Boomers approaching retirement are counting down to Medicare while juggling health costs that their current insurance may not fully protect against.
Why Underinsurance Matters
Understanding who is underinsured is critical because of the real-world consequences. Being uninsured or underinsured creates barriers to getting timely health care. Surveys consistently show that underinsured individuals behave a lot like the uninsured when faced with big bills – they delay or skip care. In one recent study, 57% of underinsured working-age adults said they did not get needed health services because of cost. This included avoiding going to the doctor when sick, not following up on recommended tests, or not filling prescriptions due to expense. When people postpone care, minor health issues can turn into major problems. In fact, about 41% of adults who delayed care for cost reasons reported that their condition worsened as a result.
Another consequence is medical debt. Underinsured families often end up with hefty bills if a health crisis strikes. Nearly 30% of underinsured adults in 2024 reported they were burdened with medical debt, and about half of those owed $2,000 or more. Such debt can damage credit, drain savings, and cause significant stress. People sometimes resort to crowdfunding their medical bills or putting expenses on high-interest credit cards. It’s a vicious cycle: underinsurance leads to debt, and fear of debt leads people to avoid further care, potentially exacerbating health issues.
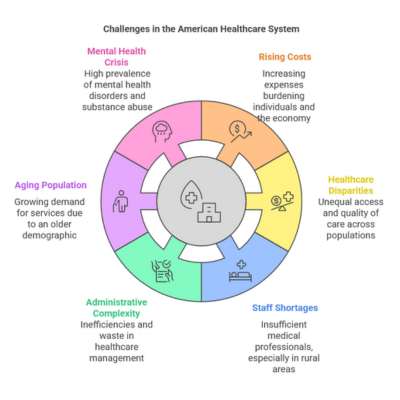
Importantly, underinsurance also highlights gaps in the insurance system. The ACA greatly reduced the number of uninsured across all age groups, especially for low-income and young adults. But the rise of high-deductible plans means the underinsured population has remained stubbornly high. This indicates that policy efforts have succeeded in getting people “insured,” but affordability of care remains a challenge. Experts often point out that the U.S. healthcare system has a dual problem now – the uninsured, and the underinsured. Any discussion about improving health coverage has to address not just expanding coverage but also making existing coverage more comprehensive and affordable.
Closing Thoughts
The health insurance gap in America is no longer just about those with no insurance, but increasingly about those with insufficient insurance. The data shows a clear pattern: lower-income Americans and people in their late 50s/early 60s are most likely to be underinsured, though a significant share of younger and middle-income folks are affected as well. In practical terms, being underinsured can mean skimping on care or facing financial distress despite paying for an insurance plan.
From a generational perspective, each age group faces its own hurdles. Millennials and Gen Z may have coverage due to the ACA, but many are in gig jobs or high-deductible plans that don’t fully shield them from costs. Gen X and late Boomers in their 50s-60s often have more health needs and see underinsurance peak just before Medicare eligibility. The common thread is that income level heavily moderates these experiences – higher-income individuals have more cushion, while those living paycheck-to-paycheck are hit hardest by high deductibles or surprise bills.
In a neutral view, addressing underinsurance is about ensuring that having health insurance actually translates into access to care. Policymakers measure progress not just by the uninsured rate, but also by metrics like how many Americans skip care due to cost or incur catastrophic medical expenses. Those metrics suggest there is more work to be done. For readers, the takeaway is to be aware of what underinsurance is and which groups are most affected. If you have insurance, it’s wise to assess: Would I be able to afford care if I got seriously ill under this plan? If the answer is no, you’re unfortunately not alone – and understanding the scope of America’s underinsured population is the first step in fostering informed discussions about how to close this remaining coverage gap